"CASE OF 42YEAR OLD FEMALE WITH
MULTIPLE HEALTH EVENTS SINCE BIRTH"
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
INTRODUCTION:
Following is my analysis of this patient's problem:
CHIEF COMPLAINTS:
•Frequent falls to the left following migraine with aura
•Fatigue following stress or exercise
•Swelling(face and abdomen)
•Hair loss (head and eyelashes)
•Breathing difficulties
•Sleepl disturbances
Elaborating each complaint in detail :-
MIGRAINE WITH AURA :
Onset - Sudden
Duration - Since 2 years of age so approximately 40 years
Progression - gradually progressive in intensity
Site - More in the left side
Associated complaints -
preceded by Aura,
generally associated with numbness of left hand and left face
feeling of rotation and spinning while sleeping on left side.
Relieving Factors - Triptans
Possible Diagnosis
- HEMIPLEGIC MIGRAINE
- Transient Ischemic Attack (
- Infections like meningitis, encephalitis (associated with a fever, rash)
- Brain tumours
- Seizures with post-ictal paralysis
- Metabolic Disturbances like Homocystinuria
- MELAS ( Mitochondrial Encephalopathy Lactic Acidosis and Stroke like episodes)
In order to confirm the above diagnoses, the possible investigations needed would include:
- CT and MRI of brain can confirm brain tumours, stroke, TIA
- CSF analysis to diagnose infections
- EEG to detect seizures
- Magnetic Resonance Angiography to diagnose TIA
- Intracranial pressure Possible treatment modalities are
- migraine - Triptans (which she is already consuming)
- Surgery (Carotid endareterectomy) - TIA ( cannot give anticoagulants because she has G6PD Deficiency)
- Anti epileptics - Seizures
RECOMMENDED TREATMENT:
Acute treatment
Triptans and ergotamines are currently contraindicated in the treatment of hemiplegic migraine because of their vasoconstrictive properties (risk of vessel spasm) and concerns about stroke. Other treatments such as NSAIDs, antiemetics, and sometimes narcotic analgesics are used for symptomatic relief of hemiplegic migraine. Intranasal ketamine has been shown to shorten the duration of aura symptoms in patients with hemiplegic migraine.
Preventive treatment:
Given the severity of the symptoms and the contraindication of certain acute medications (triptans and ergotamines), preventive regimens (medications taken daily to prevent the attacks whether you have a headache or not) are considered especially important in the treatment of hemiplegic migraine. There are small studies reporting use of verapamil, acetazolamide, flunarizine, ketamine, lamotrigine and naloxone for treatment of hemiplegic migraine. Since hemiplegic migraine is a subset of migraine with aura, certain preventive medications commonly used to treat typical migraine with aura, including amitriptyline, topiramate, and valproic acid may be beneficial. Beta-blockers are generally avoided for people with hemiplegic migraine out of theoretical concern that it may affect the ability of vessels to dilate.
FATIGUE FOLLOWING STRESS OR EXERCISE:
Aggrevated on exertion
Relieved on rest
POSSIBLE CAUSES -
Hemolytic anemia
G6PD deficiency
Adenosine monophosphate1 deficiency
Starving
( Since the patient has both G6PD-DEFICIENT and AMPD the symptoms to oxidative stress and depleted energy supplies are more severe.)
Past history shows parents to be chain smokers which increases the oxidative stress.
Treatment given
Ribose - helped her because it provides ATP.
RECOMMENDED TREATMENT
Drink lots of fluid to avoid fatigue
Drugs like modafinil, methylfenidate, amphetamine, amantadine etc are also in use .
SWELLING:
Since 1 year of age till date
Site - Face , Abdomen
Aggravating Factors-Emotional Stress, Eating wrong food such as Fava beans, Exercise, Smoke
Relieving Factors - Rest
Associated factors - Shortness of breath, Decreased urination(increased on fasting), Dark coloured urine on exercise

Possible causes for swelling:
•Right Heart Failure which is responsible for ascites and shortness of breath (because of Pulmonary artery hypertension).
•Kidney infection because G6PD is responsible for production of NADPH. And since she has deficiency of G6PD, She does not have enough NADPH and ATP which resulted in loss of lots of ions thereby causing decrease in urination and Facial edema.
•It increased on emotional stress and eating fava beans because she has G6PD Deficiency.
•Her shortness of breath could also be attributed to hiatal hernia.
•Dark urine on exercise is suggestive of hemolysis which could be due to G6PD deficiency.
Differential diagnoses :
Angioedema
Pancreatitis
Investigations done in this case are :
Hemogram - shows anemia
ECG - signs of Right Heart Failure
CXR - Left atrial enlargement in this case
SGPT, SGOT - elevated in this case suggestive of hemolysis
CUE - to show infection
Further investigations required are :
LDH -should be elevated To detect hemolysis
Total BIlirubin - should be elevated
Reticulocyte count - elevated
Urobilinogen
Heinz bodies in RBC on complete blood film
Beutler fluoroscent spot test - rapid test that identifies NADPH production by G6PD under UV Light
Haptoglobin ( decreased in hemolysis)
Direct Coomb's test - negative (suggestive of non autoimmune hemolytic anemia)
G6PD test
Skin tests for allergy (for angioedema)
RECOMMENDED TREATMENT :
Avoiding stress
Do not consume fava beans, sulpha drugs, antimalarials
Serine- increased urination
Excess salt consumption
SLEEP DISTURBANCES:
Present since birth
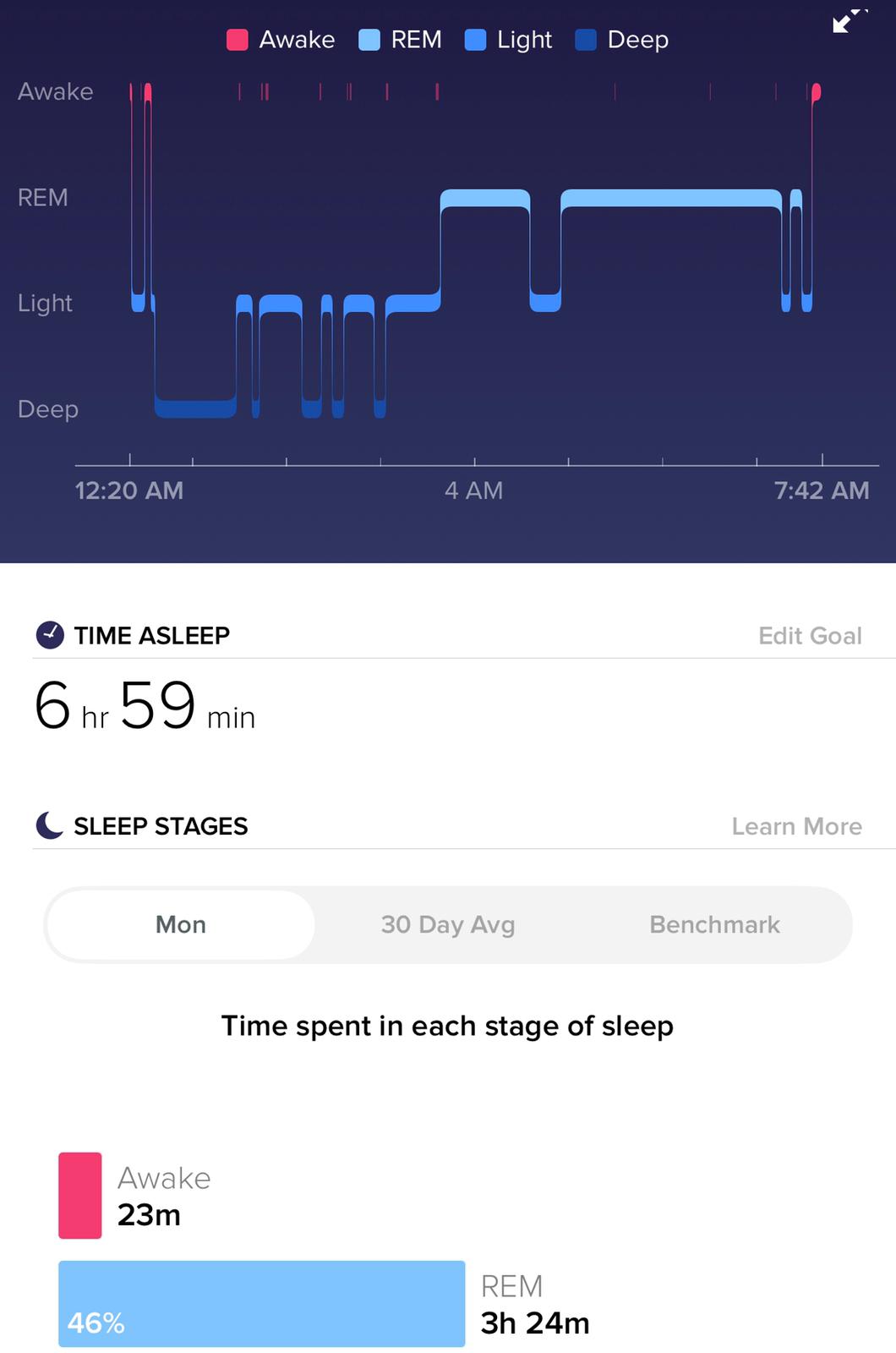
Duration of sleep - 2-4 hours and no REM sleep
Possible causes :
The lactic acidosis with palpitation may also occur during sleep, if stomach emptying has been delayed e.g. due to digestion requirements of the food or its high volume, and the person went to sleep before absorption has started. In this case the person will be awaken in a state of distress, with rapid breathing. The person may recall seeing a nightmare.
AMPD1 Deficiency can cause sleep disturbances because Adenosine is an inhibitory neurotransmitter so it should help in sleep.
G6PD Deficiency impaired the glycolysis so glycine is not formed well . Glycine is also an inhibitory neurotransmitter.
Treatment taken by her :
L serine : works like glycine in brain so helps in better sleep
Cimetidine
BREATHING DIFFICULTIES:
High glycemic index food leads to dumping of lactate which leads to Tachypnoea, Delayed Gastric Emptying leading to Shock Lactic Acidosis leads to waking up at night with tachypnoea and palpitations.
Investigations to be done:
ECG
X-RAY CHEST
ANAESTHESIA AWARENESS
During past surgeries (observed even in her grandmother)
This condition has the potential to cause malignant hyperthermia, an uncontrolled increase in body temperature, and permanent muscle damage in patients with MADD.
PAST CLINICAL HISTORY:
Birth - 1 year
Kernicterus
Tongue tie and upper lip tie. (cut by surgery at age 13 or 14)
Large upper tori.
Lack of sleep (very less, 2-4 hours only once in a day and sometimes twice)
Screamed constantly.
Vomited anything aside water and very salty broth (tried breast milk and multiple kinds of formula but no benefit) Would swell up severely- particularly in face/head and abdomen.
2 Years
Delayed milestones
3 YearsBegan shaving. Excessive hair growth on face/neck/toes/ and legs.
Still only sleeping 2-3 hours.
Still ate almost nothing without getting sick
Short stature and malnourished
4 Years - Presentsuffered
Chronic UTI Kidney infections
Strep throat (doctor diagnosed)
Lung infections
Multiple sprained ankles and knees.
(hospitalized 3 times for above issues as a kid and once as an adult later).
Since being vaccinated for pneumonia at age 28 no hospitalization for lung issues.
Severe reaction to sulfa drugs (Given as infant, mother said).
Severe headaches (since age 2). Became worse with menses(at 14) and while on BC (birth control - nuva ring) at age 32 caused migraine with aura. Seen for concerns of brain tumor- no scan done was told bloodwork looked great so no need.
Potential sensory disorder-clothes felt unbearably uncomfortable- physical contact
Have higher pain tolerance, feel painful but can not focus on pain even now.
Severe mood disorder present since childhood worsened as headaches got worse - used to get extremely angry and fighting if anyone tried to force feed.
Would suddenly snap (flip out / temper tantrum) for no reason- still feel the buildup to this state of irrational anxiety/ anger/ fear and have learned to take time out or isolate herself to calm down usually precedes a swelling event or migraine.
Does not seem tied to stress- can wake up at night with a raise in heart rate (not outside norms- but a jump) with the same symptoms as when it happens awake.
Migraines entire life- interfered with school life and still have them.
12 years age - got diagnosed for cervical degeneration and scoliosis seen on x-rays for lung infection
15 year age - headache severity increased to the point unable to get out of bed- forced to go to school.
Attempted suicide. Put in managed care Diagnosed there with anorexia for refusing to eat. Tied down and tube fed nasally (would rip the tube out- food causes extreme pain and increases anxiety states). Vomited and nearly choked.
Was sent home, cured after gaining nearly 25 lbs in 2 weeks- all abdominal and face weight.
Fluctuating weight pattern due to abdominal edema.
18 year age- got married
21 year age-
Ectopic pregnancy.
Woke up during surgery (Anaesthesia awareness)
(grandmother also has history of waking during surgery) severely tipped uterus found.
After surgery, scar revision/wound debridement- again awoke during surgery.
22 year age-
chronic abdominal pain around periods. CT showed multiple ovarian cysts- diagnosed. PCOS.
23 year age-
hospitalized for 2 weeks for severe kidney infection and pneumonia at the same time.
Type aB melanoma and 4 precancerous tissues removed seen while in hospital.
24 year age- worsening migraines, ovarian cysts and pain
30 year age- broke leg while dancing- just snapped and I collapsed.
32 year age- Severe reaction to antimalarials- was in remote Ethiopia (Diarrhoea vomiting swelling felt like
Later that year got swine flu (H1N1 active) and pneumonia- was vaccinated for pneumonia with both types of vaccinations over 2 doses.
35 year age-
“failed” LASIK
Diagned Dyslexic
Diagnosed adhd/autism spectrum by therapist and psychiatrist.
Also had a history of CSF rhinorrhoea from her left nostril.
34 year age-
Migraines increased. Left hand and face began going numb
Unbearable feeling of spinning for 2weeks
Headaches increased and aura intensified .This happened on and off.
About a month later after first spinning event- had the worst headache ever and lost vision- began stuttering.
Aura description - It always starts as a small Flicker in the upper left and then eventually becomes a crescent that covers the entire center of my vision.
Rashes on Face (Usually 2-4 times a year. Past 6 months have not had one.) Usually come with other issues and at the same time warts and EBV reactivate.


Got genetic test last year having seattle type G6PD deficiency and AMPD1 Deficiency.
INVESTIGATIONS DONE:
Heart Rate from a recent normal day :Normal
Sleep cycles..after serine administration
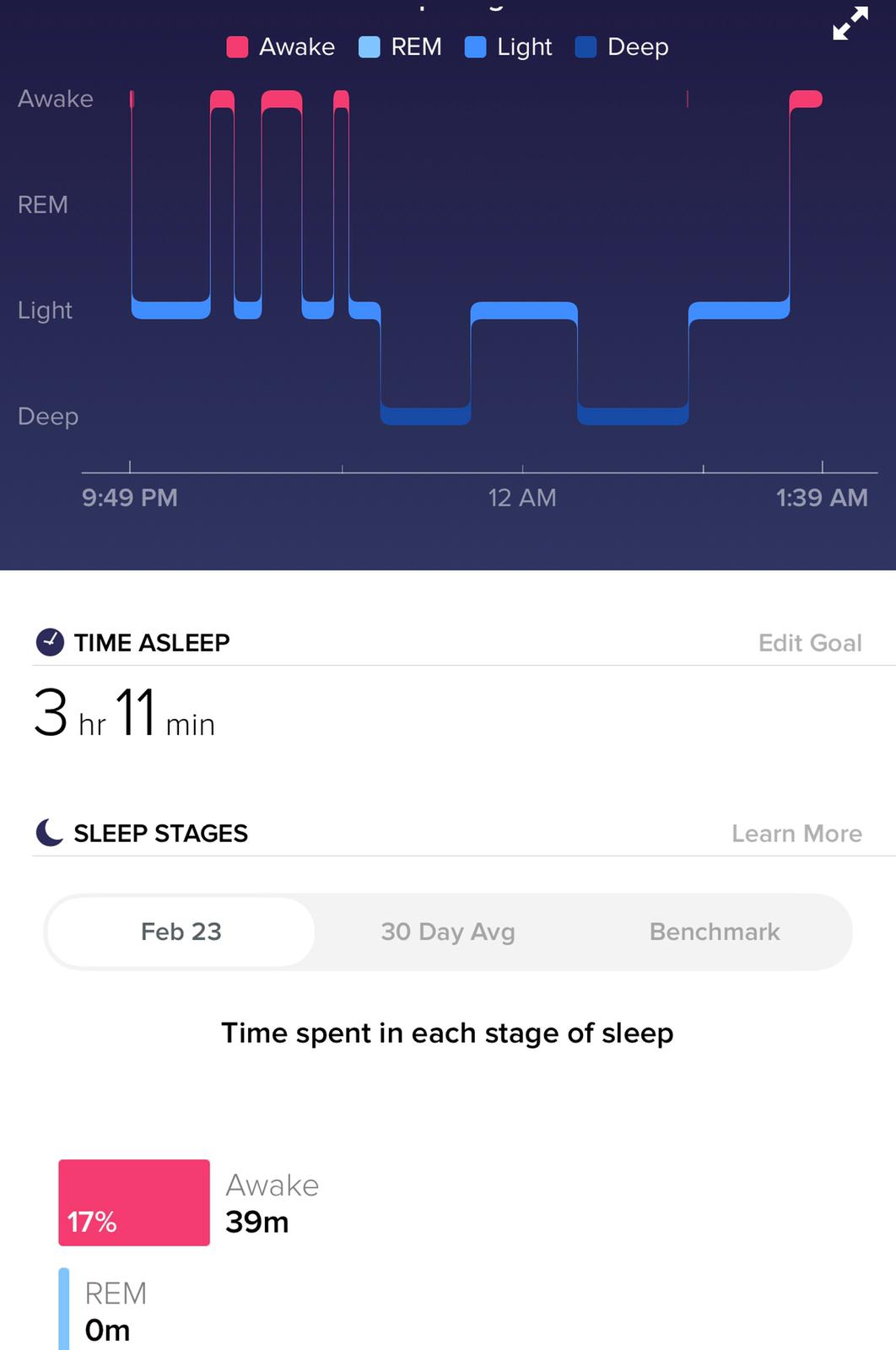
On 1st day L-Serine
EDEMA CHANGES
Edema changes within a week

1 week apart

1week apart

1 Day apart

1 week apart

Infant (frontal bossing showing high ICP?)

MRI CT Spine

Fracture (Broke other ankle again last June after falling. Was put in walking boot.)

Cortisol 2 years back - High DHEAS always , High 17-hydroxypregnenolone, other androgens are normal

FAMILY HISTORY
Mother and Dad were on spectrum ,but not diagnosed/treated.
Mother was diagnosed for fibromyalgia.
Father had heart attack in 40s.
Grand father had early death.
Grandmother had similar medical issue of anesthesia awareness also had hyperelastic skin.
GENETICSTUDIES
Seattle type G6PD deficiency
AMPD1 - AMPD1 deficiency heterozygous
MTHFR - homozygous for C677T of MTHFR = 10-20% efficiency in processing folic acid = high homocysteine, low B12 and folate levels
WNK1 mutation
HLA-DRA - 3x higher risk for developing a peanut allergy In populations of European ancestry
VWF - association with Von Willebrand disease type 1
DIO2 - 1.3-1.79x risk of osteoarthritis, 3.75x bipolar, etc.
CHRNA5 - higher risk for nicotine dependence, lower risk for cocaine dependence
ANKK1 - Tardive Diskinesia risk, higher ADHD risk. More Alcohol Dependence. Lower risk of Postoperative Nausea. Increased obesity.
TG - 1.3x to 11.5x Increased risk of autoimmune thyroid
LOXL1 LOXL1-AS1 - common but 10x higher glaucoma risk in most (but not all) populations
PNPLA3 - increased liver fat, odds of alcoholic liver disease
BACE1 - 2x increased ALZ risk in ApoE4 carriers
BSN - 1.1x risk Crohn's Disease
Increased risk for Alzheimers, ADHD, Autoimmune thyroid & other autoimmune disorders, lung cancer, cluster headache, Obesity, raised ICP, Diabetes, RA, Bipolar disorders, Lung cancer and issues,
PHARMACOLOGICAL:
Triptamines for migraine attacks
Cimetidine for Swelling, urination and sweating
Ribose to combat stress induced fatigue
Methylated B for MTHFR
Diuretics for swelling (not much useful in this case)
Food with fructose
L-serine , adenosine and cimetidine helped for enhancing sleep hours.
Iron folate supplemets for hemolytic anaemia
Antioxidant supplement pycnogenol
D- mannose and glucosamine sulfate(no effect)
Ashwagandha ,baby aspirin,amino acids showed negative effects)
Sulfur (not useful)
NAC
Nattokinase(last prescribed after being diagnosed with Behcets disease)
SURGICAL:
Tongue tie and upper lip tie (cut by surgery at age 13 or 14)
Ectopic pregnancy at 21 yrs of age during which there was Anasthesia awareness (similar to her grandmother).
Type aB melanoma and 4 precancerous tissues removed seen while in hospital at 23 yrs of age,
was hospitalized for 2 weeks for severe (worst ever) kidney infection and pneumonia at the same time.
Failed LASIK surgery at 35 yrs of age.
suffered
Chronic UTI Kidney infections Strep throat (doctor diagnosed) Lung infections Multiple sprained ankles and knees.
(hospitalized 3 times for above issues as a kid and once as an adult later)
RECENT ADVANCES IN MANAGEMENT:
✓ Cryopreservation of glucose-6-phosphate dehydrogenase activity inside red blood cells.(1)
✓Complete genome sequencing


