CBBLE UDHC SIMILAR CASES
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
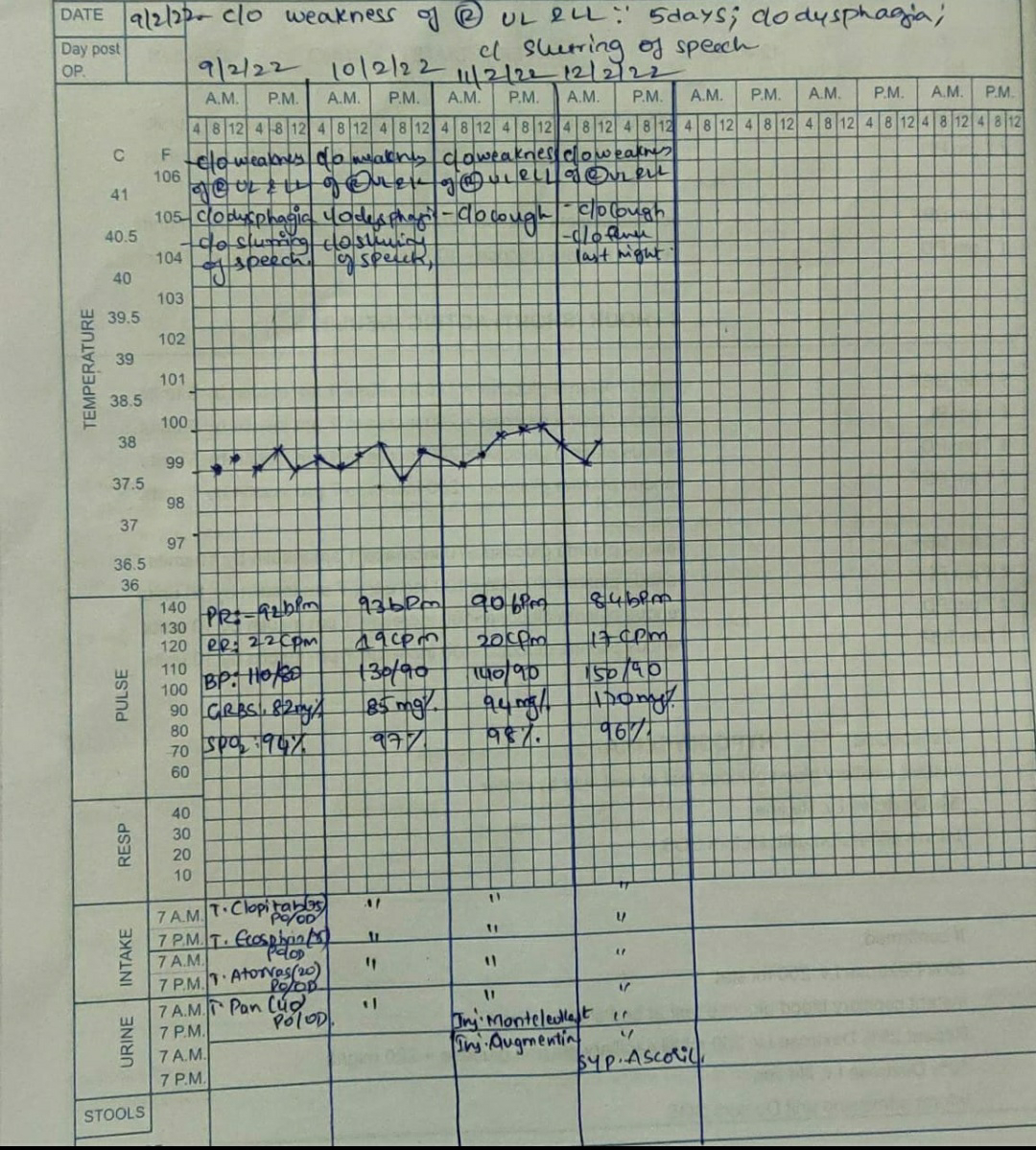
Patient was brought to casualty with complaints of deviation of mouth to right since yesterday morning,c/o slurring of speech since yesterday
HOPI:
A 90Y/M who was a farmer by occupation (staying at home since 10-15Y) Patient was apparently asymptomatic 1 yr back. Patient c/o nocturia (10-12x) overnight and went to local hospital and diagnosed with DM-2 and since then he is on regular medication .Since yesterday patient woke up from sleep. Patient complaints of deviation of mouth to right side and slurring of speech since yesterday.
Outside BP :190/100mmhg
No c/o involuntary micturition/defecation
No c/o involuntary movements
No c/o dysphagia
No c/o UL/LL weakness noted
No c/o fever,cold,cough
No c/o burning micturition since 1 month
No c/o sob, orthopnea
PAST HISTORY
k/c/o diabetes since 1 year and on regular medication since then
Not a k/c/o HTN/CAD/TB/BA
No past surgical history
PERSONAL HISTORY:
Married
Previously farmer
Appetite: Normal
BowelsBladder movements: Regular
Addictions:
Alcohol consumption (Occasional -90ml)
Had habit of smoking but stopped 5yrs ago
No other addictions
FAMILY HISTORY: Not significant
O/E :
Pt is c/c/c ,well oriented to time,place, person.
Pallor +
No signs of icterus, clubbing, cyanosis, lymphadenopathy, pedal edema.
Vitals:
Temp: Afebrile
Pr: 62bpm
Rr:17cpm
Bp:160/90 mmhg
Spo2: 97% on ra
Grbs:129mg%
Systemic Examination:
Cvs:S1S2 heard, no murmurs heard
Rs: BAE+ ,NVBS heard
P/A: Soft, nontender
CNS:-
pt conscious with Slurred speech
No signs of meningeal irritation
RIGHT LEFT
1) TONE UL NORMAL NORMAL
LL NORMAL NORMAL
2) POWER UL 5/5 5/5
LL 5/5 5/5
3) HANDGRIP 100%
4) REFLEXES
a) BICEPS + +
b) TRICEPS + +
c) SUPINATOR + +
d) KNEE + +
e) ANKLE - -
f) PLANTAR Mute Mute
5) CEREBRAL SIGNS:
Finger nose coordination: +
Knee heel in coordination: +
Sensory system:- unable to examine
Investigations:-
HEMOGRAM
HB: 10.9
TLC: 4200
N/L/E/M/B:74/18/2/6/00
PCV: 31.5
MCV: 95.3
MCH: 33.1
MCHC:34.7
RBC:3.31
PLT:1.74
RDW-CV :15.8
RDW-SD: 57.2
PS: NC/NC
BGT:- B POSITIVE
RFT:
BLOOD UREA : 30MG/DL
SERUM CREATININE: 1.1
URIC ACID:4.4
SERUM ELECTROLYTES:
Na+ : 139
K+: 2.7
Cl-: 99
LFT
TB: 1.19
DB: 0.28
SGOT:34
SGOT:10
ALP: 124
TP:5.8
ALBUMIN:3.81
A/G: 1.91
SEROLOGY: NEGATIVE
HBA1C : 6.8
FBS:141
PLBS: 94
CXR:-
ECG:-
2D ECHO:-https://youtu.be/XwX7t-Engh0
Imp:-
-Trivial TR+ ; no MR/AR
-No RWMA/No MS/AS ; sclerotic AV
-Good LV systolic function
-Diastolic dysfunction + ; No PAH/PE
MRI brain (16/2/22):-
Imp:-
-Acute Lacunar infarct in right corona radiata
-Old Lacunar infarcts in left thalamus and left corona radiata
-Chronic small vessel ischaemic changes
Carotid Doppler:(17/2/22):-
Provisional diagnosis:-
Acute ischemic CVA with UMN type of left facial palsy with acute infarct in right insular cortex.
Plan:-
1)Tab.clopotab 75mg po od
2)Tab.Ecospirin 75mg po od
3)Tab.atorvad 20mg po od
4)Inj.optineurin 1amp in 100ml Ns iv/od
-MRI Brain